Best Anxiety Disorders Medical Treatments Options That Actually Work
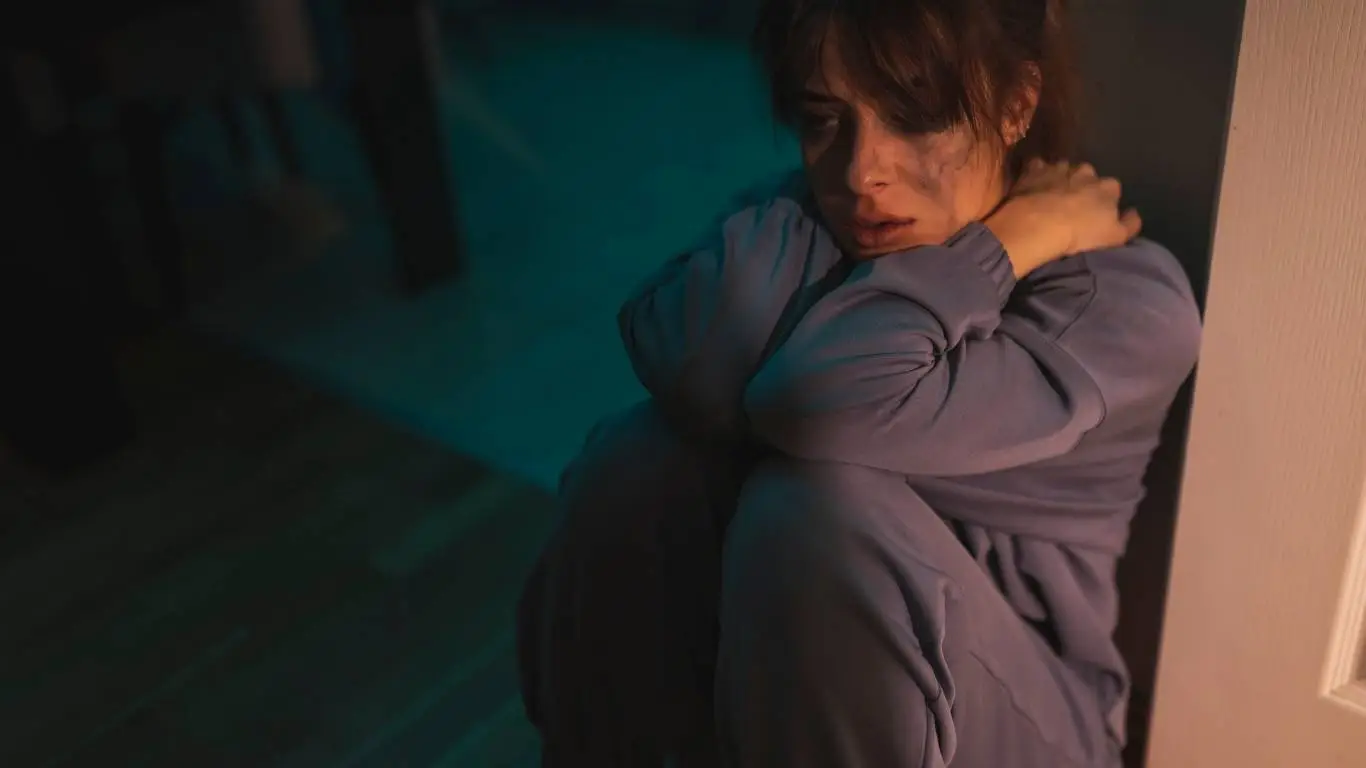
Back when I first started dealing with anxiety, I thought I just needed more sleep or a little less caffeine. I didn’t realize that what I was feeling—constant chest tightness, irrational fear of daily tasks, and this odd detachment from reality—had a medical name and actual, research-backed treatments. It wasn’t until a doctor finally said, “You’re dealing with an anxiety disorder,” that I began understanding what was really happening inside my body and brain. If you’re in the same boat, wondering whether anxiety needs more than self-help books and deep breathing, you’re in the right place.
Understanding Medical Treatment for Anxiety Disorders

When anxiety becomes persistent, disrupts your routine, or starts interfering with your relationships or work, medical intervention often becomes necessary. These aren’t just mood issues—they’re clinical conditions that can be effectively treated with evidence-based tools. Anxiety disorders, including Generalized Anxiety Disorder (GAD), Panic Disorder, and Social Anxiety, are recognized by the National Institute of Mental Health (NIMH) as serious medical conditions that deserve proper care.
Medical treatment isn’t about numbing emotions—it’s about resetting your system so you can function. For many, it’s what creates the mental space needed to even start healing.
Types of Anxiety That May Require Medical Intervention
- Generalized Anxiety Disorder (GAD): Constant worry that spans multiple areas of life, often without a clear trigger.
- Panic Disorder: Recurrent, unexpected panic attacks with intense physical symptoms like chest pain, rapid heartbeat, and shortness of breath.
- Social Anxiety Disorder: Debilitating fear of social or performance situations, often leading to avoidance behaviors.
- Obsessive-Compulsive Disorder (OCD): Repetitive, intrusive thoughts (obsessions) followed by ritualistic behaviors (compulsions).
- Post-Traumatic Stress Disorder (PTSD): Anxiety that follows traumatic events, with symptoms like flashbacks and hypervigilance.
Prescription Medications: What Doctors Actually Prescribe

The most common medical treatment for anxiety disorders is prescription medication. These aren’t quick fixes, but for many people, they are essential for regaining balance. There are several classes of drugs commonly prescribed for anxiety, each with its own mechanism and use case. Your doctor might start with one based on your symptoms, medical history, or even how fast you need relief.
1. SSRIs (Selective Serotonin Reuptake Inhibitors)
SSRIs are often the first line of treatment. They increase serotonin levels in the brain, which helps stabilize mood and reduce anxiety over time. Common options include:
- Sertraline (Zoloft)
- Escitalopram (Lexapro)
- Paroxetine (Paxil)
They typically take a few weeks to become effective. Side effects like nausea, sleep disturbances, or sexual dysfunction may occur but often subside with time. These medications are widely researched and considered safe for long-term use under medical supervision.
2. SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors)
Similar to SSRIs but also affect norepinephrine. These are often used when SSRIs aren’t effective enough:
- Venlafaxine (Effexor XR)
- Duloxetine (Cymbalta)
SNRIs may be more stimulating and can sometimes help with physical pain symptoms that overlap with anxiety, such as muscle tension.
3. Benzodiazepines
These are fast-acting medications typically used for short-term or as-needed relief. They work by enhancing the effect of a neurotransmitter called GABA, which promotes calm:
- Alprazolam (Xanax)
- Clonazepam (Klonopin)
- Diazepam (Valium)
While effective, they come with a high risk of dependence and are not recommended for long-term use. Most doctors prescribe them cautiously and only for acute situations like severe panic attacks.
4. Beta-Blockers
Though not psychiatric drugs, beta-blockers like Propranolol can reduce the physical symptoms of anxiety—especially in performance-based scenarios like public speaking. They slow heart rate and reduce shaking, without affecting mood directly.
5. Buspirone
This anti-anxiety medication is less sedating than benzodiazepines and has lower dependency risks. It’s used for long-term anxiety management and doesn’t have the withdrawal issues that benzos can bring. It’s particularly effective for generalized anxiety and can be used alongside SSRIs or SNRIs.
Medical Monitoring and Follow-Up Are Non-Negotiable

Getting a prescription isn’t a set-it-and-forget-it deal. Proper anxiety treatment includes regular check-ins with your healthcare provider. Dosages may need tweaking, side effects monitored, and sometimes a change in medication is necessary. It’s a process—not a single decision.
Most doctors follow evidence-based guidelines, often starting with lower doses and adjusting over time. You may also need basic lab work before starting certain medications. That’s not overkill—it’s just smart, comprehensive care. And always, any decision about medication should involve a licensed medical provider—not a guess based on a Reddit thread or TikTok trend.
The National Center for Biotechnology Information (NCBI) provides a thorough overview of the latest clinical approaches to treating anxiety, for those who want to go deeper into the science.
Combining Medication with Clinical-Grade Care

In most cases, medication works best when combined with other clinical treatments like therapy or psychiatric counseling. But unlike lifestyle changes, which are more preventive, medication is reactive—it tackles the biology directly. That makes it a vital pillar in many treatment plans, especially for moderate to severe anxiety cases.
For a deeper understanding of how anxiety affects daily life and why it often requires a layered treatment approach, check out the full article here: Why Anxiety Disorders Can Secretly Control Your Daily Life.
I didn’t realize how complex anxiety treatment could be until I was sitting across from my psychiatrist, completely overwhelmed by the number of medication options and unfamiliar terms. I expected a quick answer—maybe a pill, maybe a follow-up—and instead I got a deep-dive into how medications interact, what might work, what probably wouldn’t, and why managing anxiety medically is a balancing act, not a one-shot fix. If you’re exploring options or just trying to make sense of a recent prescription, let’s break it down in plain language.
How Doctors Decide Which Anxiety Medication to Prescribe

Choosing the right medication isn’t as simple as picking the strongest one. Every anxiety case is different, and your doctor is looking at several factors before writing that script. This includes:
- Your symptom profile: Is it constant worry, sudden panic attacks, physical restlessness, or obsessive thoughts?
- Medical history: Pre-existing conditions like heart problems or past adverse reactions to medications matter.
- Family history: If a close family member responded well to a certain medication, that’s a strong clue.
- Other medications: Drug interactions are a big deal—SSRIs and NSAIDs, for example, can increase bleeding risks.
- Speed of relief: Some meds take 4-6 weeks to fully work. Others, like benzodiazepines, kick in within an hour.
My doctor explained it like tailoring a suit—it has to fit you, not someone else. Even two people with the same diagnosis might end up with completely different treatment plans.
What to Expect When Starting Medication
The first few weeks can feel a little weird. You may not feel better immediately, and in some cases, symptoms can intensify before they settle. Here’s a rundown of what might happen during the adjustment phase:
- Mild side effects like nausea, headaches, dizziness, or sleepiness
- Changes in appetite or sex drive (especially with SSRIs)
- Delayed therapeutic effect—often 2 to 4 weeks before you notice a real difference
One mistake I made? Quitting too soon. I didn’t know it was normal for the first week to feel a little off. Thankfully, my psychiatrist warned me not to judge the process too early. Having that info up front can make all the difference.
What Happens If the First Medication Doesn’t Work?
About 30–40% of people don’t respond to the first medication they try. That’s not failure—it’s just chemistry. Your doctor might increase the dose, switch to a different class, or consider combination therapy. There’s a method to the process, even if it feels frustrating at first.
Augmentation Strategies
If the first line of medication isn’t cutting it, your psychiatrist might add one of the following:
- A low-dose antipsychotic like aripiprazole (Abilify) to boost the SSRI effect
- Buspirone as an adjunct to SSRIs or SNRIs
- Bupropion (Wellbutrin) to offset sexual side effects or low energy
These strategies are common in treatment-resistant anxiety and usually involve close monitoring. The goal isn’t more meds—it’s smarter combinations that target your brain’s chemistry more precisely.
Gene Testing: Does It Help?
Pharmacogenetic testing is gaining traction. Some psychiatrists use DNA swabs to see how your body might metabolize certain drugs. It’s not standard yet, but in tricky cases, it can guide more personalized treatment decisions. The latest clinical reviews suggest moderate benefits in specific contexts, though not a guaranteed roadmap.
Managing Medication Side Effects Without Quitting

Let’s be real—side effects suck. But most of them are temporary or manageable. What helps is knowing what to expect and how to respond without panicking or dropping the treatment too early.
Common Side Effects and Coping Tips
- Nausea: Take medication with food. Ginger tea and small meals can help ease stomach issues.
- Sleep disturbances: Ask your doctor if switching to morning or evening dosing helps. Some meds are activating, others sedating.
- Sexual dysfunction: This is common with SSRIs. Sometimes switching meds or adjusting the dose helps. Don’t suffer in silence—talk to your provider.
- Increased anxiety at first: Yep, it happens. This is usually temporary and subsides within 1–2 weeks.
Keeping a medication journal helped me stay objective. I tracked what I was feeling, when symptoms showed up, and how intense they were. That info made my check-ins with my psychiatrist way more productive.
Long-Term Use: Is It Safe to Stay on Anxiety Meds for Years?

This is a common concern—and a valid one. The short answer is yes, for most people, long-term use of medications like SSRIs and SNRIs is safe when supervised by a qualified provider. But like any long-term treatment, it needs regular review and monitoring.
Here’s what your provider will usually assess during long-term treatment:
- Effectiveness: Is the medication still working or has tolerance developed?
- Side effects: Are they manageable, new, or worsening?
- Life changes: Pregnancy, new diagnoses, or other meds might require adjustments.
Some people stay on medication for years and live fully functional lives. Others taper off once they’ve built coping strategies and feel stable. It’s personal—not permanent unless you want it to be.
For many, anxiety medication provides a foundation to explore deeper healing work. Once symptoms are managed, it becomes easier to engage in therapy, return to routines, and reconnect with daily life. If you’re interested in how medication ties into broader care, the main anxiety disorders overview breaks down the full picture of how anxiety affects real life.
There’s this quiet moment that hits after months on anxiety medication—when you realize your mind isn’t constantly racing anymore. For me, it was a random Tuesday. I was walking through the grocery store, not panicking, not rehearsing a million outcomes in my head. I wasn’t cured. But I was steady. That kind of progress doesn’t always come from willpower or mindset shifts alone. Sometimes it’s the result of a carefully managed medical plan. And the next question becomes: What now?
Should You Stay on Anxiety Medication Forever?

This is one of the most personal decisions you’ll face in treatment—and there’s no universal timeline. Some people stay on medication for life, while others eventually taper off. What matters is that the decision is based on your experience, not pressure from outside opinions.
Your doctor will look at a few key things before considering discontinuation:
- Stability: Have your symptoms remained well-managed for 6–12 months?
- Support: Do you have a consistent support system (therapy, relationships, coping tools)?
- Stress levels: Are you entering a calm or chaotic season in life? Timing matters.
- Previous attempts: If you’ve tried stopping before and relapsed, that experience shapes the plan.
It’s not about “dependence.” It’s about respecting the chemistry of your brain and the reality of your triggers. No shame either way.
How Tapering Off Works
Quitting anxiety medication cold turkey is never a good idea. Not only does it mess with your neurochemistry, but it can also cause withdrawal symptoms that mimic the anxiety you were trying to manage.
Here’s what a smart tapering plan usually involves:
- A slow reduction in dose over several weeks or even months
- Regular check-ins with your psychiatrist
- Monitoring for withdrawal symptoms (dizziness, agitation, fatigue)
- Having a “return” plan in case symptoms return
When I tapered off Lexapro, it took three months. I did it gradually, with tons of journaling and support. I also knew I could go back on it if things got bad again. That safety net made all the difference.
What If Anxiety Comes Back?

This part is hard to admit, but real: anxiety can return. Even with the best strategies, the right meds, and years of stability, it might creep back in. Life changes, hormones shift, grief happens, trauma resurfaces. None of that means you failed—it just means you’re human.
Here’s what you can do if symptoms start to return:
- Track the frequency and intensity—don’t ignore early signs
- Check in with your doctor right away
- Restart medication before things spiral
- Layer in therapy, even short-term, for added support
Think of anxiety management like dental care. You don’t wait for a tooth to fall out—you maintain it. Meds can be part of that ongoing maintenance. You don’t owe anyone an explanation for prioritizing your mental health.
Medical Advances in Anxiety Treatment

It’s an exciting time in psychiatric medicine. Researchers are exploring innovative options for those who don’t respond well to traditional SSRIs or want more personalized care.
New and Emerging Treatments
- Ketamine & Esketamine: Fast-acting treatments now FDA-approved for treatment-resistant depression and showing promise for severe anxiety.
- Neurofeedback: Uses real-time brainwave tracking to help you self-regulate anxious patterns.
- rTMS (Repetitive Transcranial Magnetic Stimulation): Non-invasive brain stimulation that may help rewire neural activity associated with anxiety disorders.
- Psychedelic-assisted therapy: Still experimental but gaining traction in clinical trials for treatment-resistant anxiety and PTSD under strict medical supervision.
These options aren’t first-line treatments, but they represent hope—especially for people who’ve tried “everything” and still struggle. If traditional medication hasn’t worked for you, it’s worth discussing newer options with your psychiatrist.
How to Talk to Your Doctor About Medication Options

Many people hesitate to bring up medication out of fear they’ll be judged or pushed into something they’re not ready for. But here’s the truth: any good doctor will welcome the conversation. They’re not there to pressure—they’re there to partner with you.
What Helps the Conversation Go Smoothly
- Be honest about your symptoms—don’t downplay or dramatize
- Bring a list of what you’ve tried: supplements, therapy, previous meds
- Share your goals: Do you want quick relief? Long-term management? Minimal side effects?
- Ask about risks, timelines, and alternatives—this is your body
My turning point was when I stopped seeing the doctor as someone who would “fix me” and started treating them like a teammate. We built a plan together, adjusted it along the way, and found something that worked. That mindset shift alone made me feel less powerless.
Medication Is a Tool, Not a Crutch

You wouldn’t tell someone with high blood pressure to “just relax” or someone with diabetes to “just think positive.” Anxiety disorders deserve the same respect. Medication doesn’t make you weak—it gives you the baseline strength to heal, rebuild, and function.
For those living with persistent or severe anxiety, medical treatment may be the most responsible and compassionate choice. You don’t have to suffer through it. You’re allowed to seek ease. You’re allowed to feel better. And you’re allowed to ask for help in getting there.
If you haven’t already, dive into the full picture of anxiety’s everyday impact and how medical and lifestyle approaches can work together in this detailed breakdown.

Camellia Wulansari is a dedicated Medical Assistant at a local clinic and a passionate health writer at Healthusias.com. With years of hands-on experience in patient care and a deep interest in preventive medicine, she bridges the gap between clinical knowledge and accessible health information. Camellia specializes in writing about digestive health, chronic conditions like GERD and hypertension, respiratory issues, and autoimmune diseases, aiming to empower readers with practical, easy-to-understand insights. When she’s not assisting patients or writing, you’ll find her enjoying quiet mornings with coffee and a medical journal in hand—or jamming to her favorite metal band, Lamb of God.







