Why Drug Withdrawal Anxiety Feels Worse Than You Expect
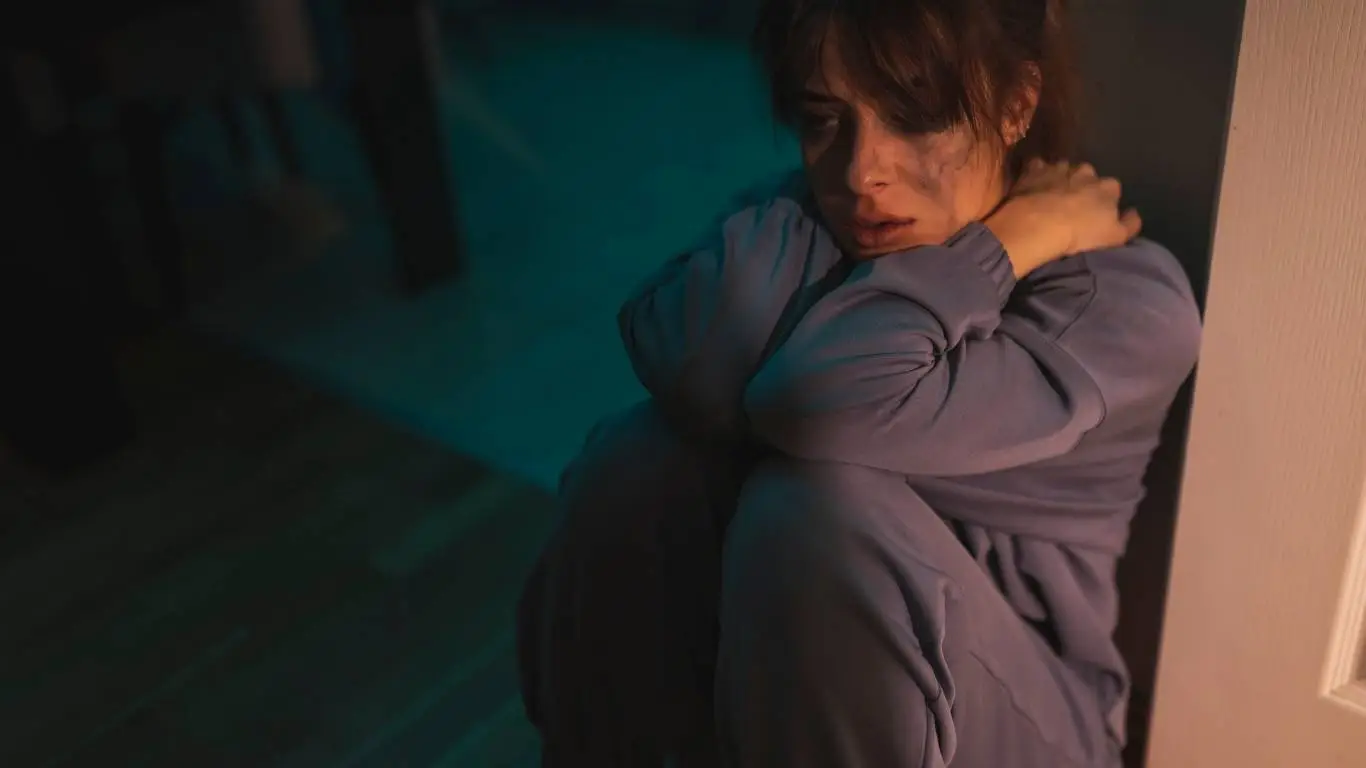
If you’ve ever felt like you’re losing control when trying to cut back on a medication, you’re not alone. Drug withdrawal anxiety is one of those things that sounds simple on paper—stop the meds, feel a little off, then bounce back. But if you’ve lived through it, you know it’s rarely that tidy. I’ve personally gone through it with SSRIs, and let me tell you—it felt like my entire nervous system was staging a protest. It’s a chaotic mix of emotions, fear, and physical symptoms that can make you question everything. Let’s get into what makes drug withdrawal anxiety so complex and how it quietly affects thousands of people every day.
What Is Drug Withdrawal Anxiety, Really?

Drug withdrawal anxiety isn’t just about missing a substance. It’s a biochemical and psychological response to the sudden absence of a drug your brain has grown used to. This doesn’t just apply to recreational substances—it’s shockingly common with prescribed medications too, especially antidepressants, benzodiazepines, beta-blockers, and even sleep aids. For many, the anxiety isn’t just a rebound of old symptoms—it’s a brand-new beast entirely.
Common Medications That Can Trigger It
- Selective serotonin reuptake inhibitors (SSRIs)
- Benzodiazepines like Xanax and Ativan
- Beta-blockers such as propranolol
- Stimulants used for ADHD treatment
- Even over-the-counter sleep aids and antihistamines
What makes this tough is how withdrawal symptoms can masquerade as a return of your original anxiety. But it’s not always a relapse—it’s your body trying to find its balance again. Benzodiazepine withdrawal, for instance, can lead to anxiety levels you never had before starting the meds in the first place.
Why Drug Withdrawal Anxiety Feels So Much Worse

Here’s the thing—withdrawal anxiety isn’t just psychological. Your brain’s neurotransmitter systems (especially GABA, dopamine, and serotonin) are in total disarray. When you suddenly stop or taper medication, it creates a neurological vacuum. The imbalance can leave you feeling agitated, dizzy, foggy, and emotionally raw. I remember pacing the floor for hours, heart pounding, thoughts racing, just waiting for the storm to pass. It’s not something a deep breath can fix.
And let’s not ignore how neurotransmitter disruptions play into this. Your brain chemistry is in a fragile state, and your nervous system interprets everything as a threat. It’s fight-or-flight on steroids.
Physical Symptoms That Mimic Other Conditions
- Heart palpitations that feel like a heart attack
- Dizziness and lightheadedness that feel like you’re going to faint
- Muscle tension and body aches
- GI symptoms—nausea, cramping, diarrhea
- Sleep disturbances that make nights feel endless
It’s no wonder some people end up in the ER thinking they’re having a medical emergency. I did—twice. And both times, it was withdrawal anxiety pretending to be something more sinister. You’re not the only one who’s been there.
The Overlooked Role of Tapering Too Quickly
We often assume that once a doctor gives the green light to stop a medication, it’s safe to do so. But tapering is an art—and rushing it can be brutal. In my case, I cut my dosage in half over a week, thinking I was doing it slowly. Bad idea. The anxiety came back with a vengeance and brought friends: insomnia, mood swings, intrusive thoughts, and an overwhelming sense of dread.
This is where proper clinical guidance makes all the difference. Some medications, especially benzos and SSRIs, require months of careful reduction under medical supervision.
Better Tapering Practices
- Decrease doses in 10% increments every 2–4 weeks
- Track symptoms daily in a journal or app
- Involve your prescribing physician in every step
- Use liquid formulations when possible for precision
- Stay hydrated and focus on anti-inflammatory foods
There’s no shame in slowing things down. In fact, that’s usually the smarter route. According to PubMed and Psychology Today, rapid tapering is one of the leading causes of withdrawal-induced anxiety flare-ups.
How to Manage the Anxiety Without Reinstating the Drug

One of the biggest traps in withdrawal anxiety is reinstating the drug just to feel normal again. And trust me, I understand why. But the goal should be to get through it without going back—unless medically advised. There are real, actionable tools that help soften the withdrawal blow.
Grounding Techniques That Worked for Me
- Progressive muscle relaxation: Simple, but incredibly effective. Here’s a guide that helped me stay grounded when my body felt out of control.
- Breathing exercises: Deep diaphragmatic breathing was my anchor during the worst of it. These techniques made a noticeable difference.
- Magnesium-rich foods: My diet became part of my recovery. Magnesium helped more than I expected.
- Journaling: It gave structure to the chaos. Noticing patterns helped me reclaim a sense of control. Seriously, journaling works.
For a complete recovery approach, don’t overlook how lifestyle and diet can ease the transition. The lifestyle/self-help pillar dives deeper into practical steps that don’t involve meds. And to understand how anxiety disorders can quietly take over everyday life—even without drugs—check out this essential main article.
When Withdrawal Anxiety Doesn’t Go Away

Let’s talk about the fear that no one really warns you about: what if the anxiety sticks around? What if weeks pass, then months, and you’re still feeling wired, panicked, or just… off? I’ve been there. I remember googling “permanent withdrawal anxiety” at 3 AM like my life depended on it. Some people recover in a few weeks. For others, it takes longer. That doesn’t mean you’re broken—it means your nervous system needs more time.
There’s even a name for it: protracted withdrawal syndrome. It’s not rare, especially with benzos and antidepressants. And unfortunately, it’s under-recognized by a lot of healthcare providers. Many doctors still misinterpret lingering symptoms as a relapse rather than the tail end of withdrawal.
How Long Can It Last?
- Short-term: 1–4 weeks – Common with mild SSRI withdrawal
- Medium-term: 1–3 months – Common with beta-blockers or sleep meds
- Long-term: 6+ months – Often seen with long-term benzo or poly-drug users
I dealt with a mild version of this for about 4 months. It was frustrating, unpredictable, and I felt like progress was constantly one step forward, two steps back. But slowly, things improved. I started sleeping again. My appetite came back. The noise in my head started to quiet down.
The Power of Non-Medication Therapies

When medication is no longer an option—or feels like a step backward—it’s time to lean into therapies that support your nervous system, not hijack it. I was skeptical at first. How could talking help when my body felt like it was burning from the inside? But the right approach made all the difference.
Therapies That Help Rewire Post-Withdrawal Anxiety
- EMDR therapy: Originally developed for trauma, but incredibly effective at calming the nervous system post-withdrawal.
- Cognitive Behavioral Therapy (CBT): Helped me break the feedback loop of fear about symptoms.
- ACT (Acceptance and Commitment Therapy): Taught me to coexist with anxiety instead of fighting it at every turn.
It’s about retraining your brain to trust that the symptoms are temporary and manageable—not dangerous. That reframing work is crucial. When your mind stops interpreting every sensation as an emergency, your nervous system starts to settle down too.
Supportive Daily Habits That Actually Help

There were days I couldn’t function, but I started building little anchors into my day. A short walk outside, journaling with a cup of herbal tea, guided meditations on YouTube—these tiny habits helped rebuild the foundation. And over time, they started to add up.
Daily Stabilizers That Kept Me Going
- Early morning sunlight exposure: Helped reset my sleep-wake cycle.
- High-quality omega-3s: Brain food. Helped stabilize my mood more than I expected.
- Yoga: Not for the workout—but for the grounding. The slow movement calmed my nervous system.
- Limiting caffeine and sugar: These made my anxiety 10x worse during withdrawal. Sugar was a bigger culprit than I realized.
What worked best wasn’t a magic bullet—it was consistency. Creating structure when my world felt chaotic made me feel safer in my own skin again.
When to Ask for Help

If you’ve been white-knuckling withdrawal anxiety alone, please hear this: you don’t have to do it solo. If the anxiety is spiraling, impacting your job, relationships, or making daily tasks feel impossible, it’s time to bring in support. Therapy, online support groups, and integrative practitioners can all offer real relief.
And if you’re not sure where to start, this guide to anxiety-focused therapy breaks down your options in a way that’s not overwhelming.
I found comfort in knowing I wasn’t alone. Other people had gone through this, and they’d come out the other side stronger. There’s something powerful about hearing, “I’ve been there too.” That validation? Priceless.
Small Wins Count—Here’s Why

When I was deep in withdrawal anxiety, the idea of being “normal” again felt impossible. But progress isn’t always big or obvious. Sometimes it’s just realizing you made it through a day without crying. Or driving again without panic. Or sleeping through the night. Those wins matter. They build momentum. They prove your nervous system is healing—even when it doesn’t feel like it.
And if you ever find yourself doubting whether you’re getting better, come back to this: You’re not your anxiety. It doesn’t get to run the show forever.

Camellia Wulansari is a dedicated Medical Assistant at a local clinic and a passionate health writer at Healthusias.com. With years of hands-on experience in patient care and a deep interest in preventive medicine, she bridges the gap between clinical knowledge and accessible health information. Camellia specializes in writing about digestive health, chronic conditions like GERD and hypertension, respiratory issues, and autoimmune diseases, aiming to empower readers with practical, easy-to-understand insights. When she’s not assisting patients or writing, you’ll find her enjoying quiet mornings with coffee and a medical journal in hand—or jamming to her favorite metal band, Lamb of God.