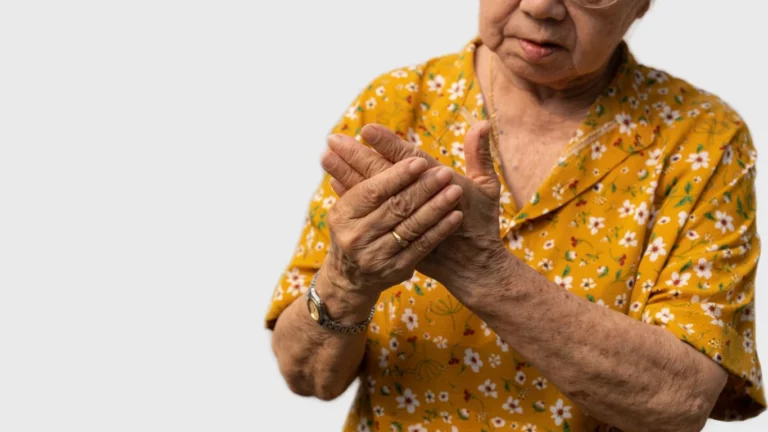
Best Ways to Prevent Arthritis Joint Deformity and Stay Pain-Free
As a rheumatology nurse practitioner who’s spent years knee-deep in swollen joints, morning stiffness, and flare-up stories, I’ve seen firsthand how critical early intervention and lifestyle adjustments can be. One of the best ways to prevent arthritis joint deformity is catching it before it sneaks up and changes someone’s entire quality of life. And let me tell you—once joint damage sets in, it’s like trying to un-toast bread. It’s not happening. So, if you’re here looking for real, practical tips (not the sugar-coated kind), you’re in the right place. I’m pulling from real-life clinic moments and trusted medical insights to help you stay ahead of the curve.
Understanding the Roots of Joint Deformity in Arthritis

Let’s start with the “why” behind joint deformity. You probably already know arthritis is a big umbrella term, but the most aggressive culprit when it comes to joint damage? That’s rheumatoid arthritis (RA). I’ve sat with countless patients who came in thinking it was just normal aging, only to find out their immune system had been quietly attacking their joints for months or even years.
When untreated or poorly managed, chronic inflammation starts breaking down the cartilage and bones in the joints. Over time, that results in visible deformity, reduced mobility, and chronic pain. What’s even scarier? It doesn’t take decades. Sometimes, damage shows up within just a couple of years.
How to Spot the Early Red Flags
So many people wait too long because they don’t recognize the subtle signs. I always tell my patients, if you’re waking up with stiffness that lasts more than an hour, or if small joints like your fingers and wrists are puffy and tender for no obvious reason, don’t brush it off. Trust me—I’ve seen folks come in saying, “It’s just because I was gardening,” and a few tests later, we’re talking about disease-modifying treatment plans.
- Prolonged morning stiffness (longer than 30–60 minutes)
- Persistent joint swelling and redness
- Fatigue that feels bone-deep and unshakable
- Loss of joint function or reduced grip strength
Recognizing these early signs can make all the difference between managing symptoms and facing long-term joint changes.
Best Ways to Prevent Arthritis Joint Deformity Through Early Action

If you’re reading this, you’re already doing one of the most powerful things you can do—educating yourself. But what next? There’s no magic bullet, but these strategies are what I walk through with nearly every patient I see. They work, and they’re backed by both experience and science.
1. Get Diagnosed—Early and Accurately
First things first: don’t self-diagnose based on Dr. Google. I’ve had patients delay proper care because they thought their symptoms didn’t “look like” arthritis. If something feels off, see a specialist. A rheumatologist can run lab work, imaging, and clinical assessments to give you a clear answer.
2. Start Disease-Modifying Medications Early
This is one of those non-negotiables. The earlier we start DMARDs (Disease-Modifying Antirheumatic Drugs), the better the chances we have at stopping joint damage in its tracks. Biologics and JAK inhibitors have come a long way. I’ve watched patients regain control of their lives within months of starting the right therapy.
- Methotrexate (often the first-line DMARD)
- Biologics like Enbrel, Humira, or Remicade
- JAK inhibitors like Xeljanz or Rinvoq
It’s not a one-size-fits-all approach. I always work with my patients to find what fits their lifestyle, tolerance, and goals best. And yes—sometimes it’s trial and error at first, but the payoff is worth it.
3. Keep Moving—Even When It’s Hard
Staying active can feel counterintuitive when your joints are angry. But movement truly is medicine. I always recommend working with a physical therapist early on—someone who knows arthritis and can guide you in safe, joint-friendly exercises.
Walking, swimming, and gentle strength training can all help maintain range of motion and protect joints from becoming stiff or misaligned. And here’s the kicker: movement actually helps calm inflammation over time.
Protecting Your Joints from Daily Damage

When patients ask me, “What can I do day-to-day to keep my hands from curling or my knees from locking?” this is where we dive into joint protection strategies. It’s not just about big medical interventions—it’s the little everyday habits that stack up over time.
4. Use Assistive Tools and Ergonomics
I’m a huge fan of adaptive tools. Jar openers, easy-grip utensils, raised toilet seats, voice-to-text software—it might sound small, but every bit of strain you take off your joints is a win. I’ve had patients who were skeptical at first but now swear by these tweaks.
- Use larger pens or grips to reduce hand strain
- Switch to lightweight cookware
- Use grab bars in bathrooms and stair rails
And don’t overlook workspace ergonomics. A proper chair, keyboard, and monitor setup can help you avoid repetitive stress injuries that accelerate joint damage.
Nutrition: A Hidden Weapon Against Joint Damage

Let me tell you—what you put on your plate matters way more than most people think. Over the years, I’ve had plenty of patients raise their eyebrows when I suggest changing up their diet, but then they come back weeks later, shocked at how much less achy and stiff they feel. When it comes to finding the best ways to prevent arthritis joint deformity, food is a sleeper strategy that deserves more attention.
Inflammation is the villain here, so we want to eat in a way that helps cool things down, not fan the flames. That doesn’t mean you have to toss all your favorite foods, but making mindful swaps and additions can make a huge difference.
Foods That Fight Inflammation
- Fatty fish like salmon, sardines, and mackerel (loaded with omega-3s)
- Leafy greens like spinach, kale, and Swiss chard
- Berries—especially blueberries and strawberries (nature’s anti-inflammatory candy)
- Turmeric (with black pepper to help absorption)
- Olive oil instead of butter or margarine
At the same time, it helps to ease off the foods that stir up inflammation—processed sugars, fried foods, and too many refined carbs are the usual suspects. I’m not saying you can’t enjoy the occasional treat, but keeping these to a minimum really does pay off in the long run.
Supplements That Might Help (But Ask First!)
Now, I’m not a big fan of loading up on supplements unless there’s a reason—but a few have shown promise. I usually talk these over with my patients to tailor them to individual needs.
- Vitamin D – especially if you’re low (which many folks with arthritis are!)
- Fish oil – those omega-3s again, in pill form if you’re not into seafood
- Turmeric or curcumin capsules – anti-inflammatory support, but make sure they’re high quality
And always—always—run supplements by your rheumatologist or primary provider, especially if you’re on meds. Interactions are a real thing.
Managing Stress to Minimize Flare-Ups

This one catches people off guard all the time. Yes, your mind can affect your joints. Stress triggers inflammatory pathways, and I’ve seen people spiral into flare-ups after tough emotional stretches—divorce, job loss, grief, or even chronic anxiety.
As a nurse practitioner, I always ask my patients about their stress levels, even if they come in for purely physical complaints. We’re not just bones and joints walking around—we’re whole humans. And stress has a sneaky way of amping up symptoms.
Simple Tools to Keep Stress in Check
You don’t have to turn into a yogi overnight, but carving out time to relax and unwind is powerful. Some options my patients have found helpful include:
- Guided meditation apps like Calm or Insight Timer
- Gentle yoga or tai chi – low impact and calming
- Daily walks in nature – no podcast, no screen, just breathe
- Talk therapy – underrated, but incredibly effective
When your body is already dealing with inflammation, the last thing it needs is a cortisol surge from unrelenting stress. Give yourself permission to rest—not just physically, but mentally too.
Staying Consistent With Care and Monitoring

Here’s something I can’t stress enough: consistency is everything. You could be on the best medication out there, eating clean, doing all the right stretches—but if you’re skipping appointments or not monitoring your disease activity, things can slip through the cracks fast.
I always encourage my patients to think of arthritis care like maintaining a car. You wouldn’t wait until your engine dies to get an oil change, right? Same deal here. Regular labs, imaging when needed, and honest check-ins with your provider help catch issues before they escalate.
What Consistent Care Looks Like
- Routine bloodwork to monitor inflammation markers and medication side effects
- Ultrasounds or X-rays to track joint health
- Medication reviews every few months (especially if on DMARDs or biologics)
- Open communication with your care team—don’t wait for a crisis to speak up
I had a patient once who faithfully tracked her symptoms in a journal and brought it to every appointment. We caught a subtle flare pattern early and adjusted her treatment before damage set in. That kind of partnership makes a world of difference.
Final Tip: Listen to Your Body
Sounds cliché, I know—but it’s something that really matters. If something feels off, it probably is. Fatigue creeping in, more joint tenderness than usual, or even changes in mood—these can all be signals that inflammation is bubbling up again.
Trust yourself, and don’t brush off those whispers from your body. You live in it every day. You know when something’s not quite right.
Empowering Your Daily Routine to Prevent Joint Deformity

In my years working with patients battling arthritis, I’ve seen how small, consistent changes in daily habits can make a significant difference in preventing joint deformities. It’s not just about medications and doctor visits; it’s about the choices you make every day.
Prioritize Ergonomic Tools and Techniques
Using tools designed to reduce joint strain can be a game-changer. For instance, ergonomic kitchen utensils and adaptive office equipment can minimize stress on your hands and wrists. I often recommend patients to:
- Use jar openers or electric can openers to reduce hand strain.
- Opt for pens with larger grips to ease writing tasks.
- Adjust computer workstations to maintain neutral wrist positions.
These adjustments, though minor, can collectively reduce the risk of joint stress leading to deformities.
Incorporate Joint-Friendly Exercises
Regular, low-impact exercises can strengthen muscles around the joints, providing better support and reducing the risk of deformity. Activities like swimming, walking, and yoga are excellent choices. According to the Mayo Clinic, these exercises help maintain joint flexibility and muscle strength without putting undue stress on the joints.
I’ve seen patients who commit to regular exercise routines experience fewer flare-ups and maintain better joint function over time.
Understanding the Role of Footwear in Joint Health

Footwear plays a crucial role in joint alignment and health. Wearing shoes that provide adequate support can prevent undue stress on the knees, hips, and back. I advise patients to look for:
- Arch support to maintain proper foot alignment.
- Cushioned soles to absorb shock.
- Wide toe boxes to prevent crowding of toes.
Proper footwear can significantly reduce joint pain and the progression of deformities, especially in weight-bearing joints.
Regular Check-Ins with Healthcare Providers
Consistent monitoring of your condition is vital. Regular visits to your rheumatologist or primary care physician can help track the progression of arthritis and adjust treatment plans as necessary. Early detection of changes allows for timely interventions, which can prevent or minimize joint deformities.
In my practice, I’ve found that patients who maintain regular appointments and open communication with their healthcare team often have better outcomes and fewer complications.
References
- Arthritis Foundation: Joint Deformities in Rheumatoid Arthritis
- Mayo Clinic: Arthritis Pain – Do’s and Don’ts
- CDC: Self-Care for Arthritis
- Healthline: Preventing Arthritis in the Hands
Disclaimer
This article is intended for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare provider for personalized medical guidance. The strategies discussed are based on general recommendations and personal experiences in clinical practice. Individual results may vary.

Tarra Nugroho is a dedicated Nurse Practitioner with a strong foundation in family and preventive care. She brings both compassion and clinical expertise to her practice, focusing on patient-centered care and health education. As a contributor to Healthusias.com, Tarra translates medical knowledge into clear, empowering articles on topics like women’s health, chronic disease management, and lifestyle medicine. Her mission is simple: help people feel seen, heard, and informed—both in the clinic and through the content she creates. When she’s not caring for patients, Tarra enjoys weekend hikes, plant-based cooking, and curling up with a good health podcast.