GERD-Safe Bedtime Routines Tips 🛏️💤
Getting a good night’s sleep with GERD isn’t just a luxury—it’s a necessity. I’ve been through the tossing and turning, the middle-of-the-night heartburn that feels like fire creeping up your chest. It’s frustrating, and honestly, it messes with more than just your sleep—it affects your energy, your focus, and your mood the next day. The truth is, small changes to your nighttime routine can make a big difference in how your body handles reflux while you sleep.
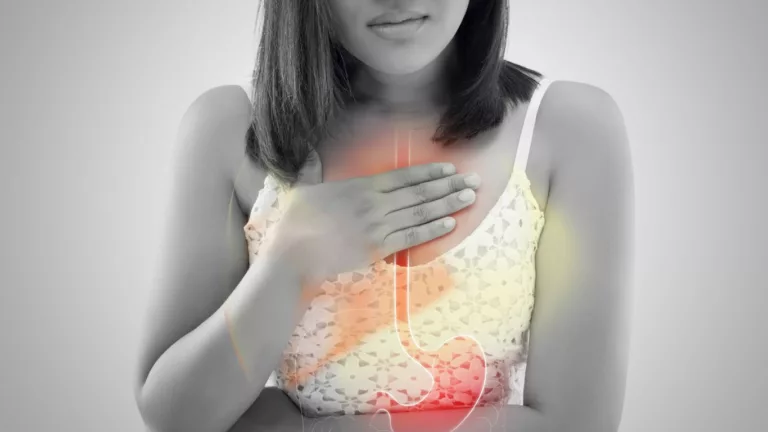
Why GERD Symptoms Worsen at Night

When you lie down, gravity no longer helps keep stomach acid in its place. For those of us with GERD, this often means acid makes its way back into the esophagus, leading to nighttime symptoms like coughing, chest discomfort, or that dreaded burning sensation. According to the Mayo Clinic, nighttime reflux can even lead to sleep disturbances, worsening the overall impact GERD has on your quality of life.
Creating a GERD-Friendly Sleep Environment

I underestimated this for years. I thought my mattress and pillow were good enough—but when I finally invested in a wedge pillow and changed the layout of my bedroom, I started sleeping better almost instantly.
1. Elevate the Head of Your Bed
Lying flat makes it easy for stomach acid to rise. Elevating your upper body—even just by 6 to 8 inches—can help keep acid where it belongs. I started with stacking pillows but quickly learned that a wedge pillow or adjustable bed base was way more effective and comfortable long-term. Learn more about this in our guide on head-of-bed elevation techniques.
2. Choose the Right Pillow
Not all pillows are created equal when it comes to GERD. Look for options specifically designed for acid reflux or GERD relief—these tend to maintain the right angle to reduce nighttime symptoms. Here’s a helpful breakdown of the best pillows for acid reflux that I found super helpful when upgrading mine.
3. Optimize Your Mattress
A firm but comfortable mattress can reduce pressure on your stomach. For me, switching from a super-soft mattress to a medium-firm one made a noticeable difference—less compression, better sleep posture.
Eating Habits That Influence Nighttime GERD

This is one area where I had to unlearn a lot. Late-night snacking, spicy takeout dinners, and sipping wine right before bed? Bad combo. If any of that sounds familiar, you’re not alone. But tweaking your dinner routine can offer massive relief.
1. Don’t Eat Too Close to Bedtime
Experts generally recommend finishing meals at least 2–3 hours before lying down. This allows your stomach time to empty. I used to eat dinner around 9 p.m. and be in bed by 10:30—until I realized that might be why I kept waking up coughing. I now aim for dinner by 6:30 or 7 p.m., and the difference has been night and day (pun intended).
2. Watch What You Eat
Skip the tomato sauce, onions, citrus, chocolate, and high-fat meals. Instead, stick to GERD-safe foods like lean proteins, steamed vegetables, and complex carbs. I’ve found that oatmeal, grilled chicken, and baked sweet potatoes keep my stomach calm before bed.
3. Stay Hydrated—But Time It Right
Hydration helps digestion, but drinking large amounts of water just before lying down can increase stomach pressure. Try sipping throughout the day instead of gulping it all down in the evening. This article on water intake and acid reflux has great tips on doing it right.
Habits That Calm the Body Before Bed

It took me a while to realize my stressed-out evenings were feeding my reflux. Now, my bedtime routine feels more like a wind-down ritual—and it’s made all the difference.
1. Incorporate Gentle Movement
Light stretching or a short walk after dinner helps digestion and reduces stress. Just don’t do anything too intense—avoid workouts within two hours of bed. Try these GERD-safe movements that promote better digestion and relaxation.
2. Try Relaxation Techniques
Practices like deep breathing, progressive muscle relaxation, or meditation can calm both your mind and stomach. I personally love putting on calming music and doing some guided meditation for reflux right before bed. It sounds simple, but it’s shockingly effective.
3. Keep a Consistent Sleep Schedule
Going to bed and waking up at the same time daily trains your body to get better rest, reducing stress and inflammation overall. And yes, weekends count too—your stomach doesn’t know it’s Saturday.
Nighttime Triggers to Avoid

Sometimes it’s not what you do—it’s what you don’t do. Recognizing and avoiding common bedtime triggers can significantly reduce your symptoms.
- Alcohol: Especially red wine—it relaxes the lower esophageal sphincter, making reflux more likely. Here’s a deep dive into alcohol’s effects on reflux.
- Smoking: If you’re still smoking, know that it’s one of the worst things you can do for GERD. Learn how smoking worsens acid reflux.
- Tight Clothing: Ditch those tight pajamas or waistbands. Clothing that compresses your abdomen can push acid upward—something I only realized after sleeping in old yoga pants one night and waking up in pain.
If you’re serious about improving your GERD symptoms holistically, I also recommend checking out our comprehensive guide on lifestyle changes for GERD relief. Small steps, big difference—especially when it comes to bedtime routines.
Choosing the Right Bedtime Snacks (If You Must)

Let’s be real—sometimes we get hungry before bed. Skipping a snack can make reflux worse if your stomach gets too empty. I’ve had those nights where I tried to power through and ended up with that awful gnawing burn in my chest. The trick is picking the right snack that doesn’t wake the acid dragon.
What to Eat if You’re Hungry
- Low-fat yogurt: Choose unsweetened or low-sugar varieties.
- Banana with almond butter: Easy on the stomach and gently filling.
- Plain oatmeal: A small bowl can absorb acid and keep you full.
- Whole-grain toast with a light spread: Avoid butter or citrus jams.
If you’re unsure which snacks won’t trigger symptoms, this guide on low-fat GERD-safe snacks can help you stock your pantry wisely.
Snacks to Avoid Before Bed
Even a “tiny” bite of the wrong food can haunt you for hours. I’ve made the mistake of grabbing a handful of chocolate or leftover pizza—and regretted it around 2 a.m.
- Chocolate
- Spicy chips or crackers
- Cheese-heavy foods
- Mint or peppermint candies
Remember, even healthy foods like citrus fruits or tomato-based items can trigger reflux. Check out this helpful breakdown on spices and flavorings safe for GERD.
Sleep Position Matters More Than You Think

This one changed everything for me. I used to sleep flat on my back thinking it was the “neutral” position. But once I started consistently sleeping on my left side, my nighttime symptoms dropped dramatically.
Why Left Side Sleeping Helps
There’s actual science behind this. Sleeping on your left side keeps the stomach below the esophagus, minimizing acid exposure. A study published in the Journal of Clinical Gastroenterology showed that left-side sleeping can reduce reflux episodes significantly compared to the right side.
Positions to Avoid
- Right side: This position relaxes the lower esophageal sphincter and worsens reflux.
- Back sleeping: Unless you’re using an elevated wedge pillow, acid can pool more easily.
- Stomach sleeping: Adds pressure to your abdomen and esophagus—major trigger.
We explore this further in our breakdown on the best GERD-safe sleeping positions.
Bedroom Environment Tips for Better Sleep

It’s not just about what you eat or how you sleep—your bedroom itself plays a big role in how well you rest. Over the years, I’ve turned my room into a reflux-friendly sanctuary and it’s been a game-changer.
Keep It Cool and Dark
A slightly cooler room—around 65°F (18°C)—helps signal your body it’s time to rest. Use blackout curtains if street lights or early sunrises tend to wake you too early.
Use a Humidifier if Needed
Dry air, especially if you mouth-breathe or have sinus issues, can irritate your throat lining—already sensitive from reflux. I found that adding a small humidifier reduced that scratchy morning throat sensation.
Avoid Blue Light Before Bed
Put your phone down at least 30 minutes before sleep. That endless scrolling not only delays sleep but also increases stress—which can aggravate reflux. Try reading instead (preferably something relaxing, not your to-do list!).
Evening Routines That Soothe Your Stomach

One of my favorite rituals? A warm (not hot!) herbal tea, a quick gratitude journal, and some quiet breathing. It sounds basic, but these little actions set the tone for sleep and give my digestive system a chance to settle.
Herbal Teas That Don’t Trigger GERD
Skip peppermint—it relaxes the esophageal sphincter. Instead, go for:
- Chamomile tea (learn more about its benefits here)
- Ginger root tea
- Fennel or marshmallow root (great if your throat feels irritated)
Journaling or Light Reading
Putting thoughts on paper clears your mind—and helps you avoid mentally digesting the day while your body’s trying to rest. If you need something to read, try a topic that’s interesting but not stimulating—nothing true crime or financial planning!
Gentle Yoga or Stretching
I love this routine: child’s pose, knees-to-chest, and some neck rolls. Helps settle your core and relieves tension in the upper chest and throat. You can explore more ideas in our GERD-friendly yoga guide.
Monitor What Works for You

Everyone’s body is different. What works for me might not work for you—and that’s okay. Start tracking your sleep habits, your meals, and how you feel when you wake up. Over time, patterns will emerge, and that insight is powerful.
I recommend using a simple journal or phone note to track:
- What and when you eat
- Your bedtime and wake-up time
- Reflux symptoms during the night
- Any stressful events or triggers that day
This reflective practice helped me identify things I would’ve never guessed were triggers—like having dinner too late, or drinking even a tiny bit of citrus tea at night.
For a broader understanding of GERD symptoms and triggers, check out our pillar article on GERD symptoms you shouldn’t ignore.
What to Do When Nighttime Reflux Strikes Anyway

Even with the best bedtime routine, there are nights when GERD still flares up. I’ve had those frustrating wake-ups at 2 a.m., heartburn blazing, wondering what went wrong. The key is to have a few reliable strategies in your back pocket so it doesn’t spiral into a sleepless night.
1. Sit Up, Don’t Lie Back
If you’re hit with reflux mid-sleep, prop yourself upright or sit in a recliner. Gravity is your ally here. Lying flat again only makes the acid situation worse.
2. Sip Warm Water or Herbal Tea
Sometimes a few sips of warm chamomile or ginger tea can soothe the esophagus and calm things down. Avoid milk—it can feel soothing at first but may worsen symptoms later for some.
3. Chew Gum to Stimulate Saliva
Chewing sugar-free gum helps stimulate saliva, which neutralizes acid. I keep a pack by the bedside just in case. Just skip anything minty—mint can relax the LES and make things worse.
4. Avoid Antacids as a First Resort
Unless your symptoms are severe or persistent, avoid jumping straight to medication every time. Frequent use of antacids can mask patterns and delay addressing the real root causes. But if you need quick relief, products like Gaviscon or low-dose H2 blockers may help in moderation.
When to Talk to a Doctor About Nighttime GERD

If your GERD symptoms continue to disturb your sleep more than twice a week, it’s time to speak up. Don’t wait until you’re constantly fatigued or developing complications. I wish I had been more proactive about this years ago.
Signs You Need Medical Support:
- Persistent cough or sore throat in the morning
- Regurgitation or vomiting at night
- Choking or gasping awake (possible silent reflux or LPR)
- Chest pain that mimics heart attack symptoms
- Heartburn despite routine and medication
Your doctor might recommend advanced testing, like a pH monitoring study or endoscopy, or adjust your treatment plan with PPIs or other long-term solutions. Learn more about diagnostic options in our article on GERD diagnosis methods.
Smart Lifestyle Tweaks That Reinforce Better Sleep

Once I committed to changing more than just my sleep routine—like how I handled stress and my daytime eating habits—my nighttime GERD improved even further. It really is all connected.
Focus on These Daytime Habits:
- Eat smaller, more frequent meals: Reduces pressure on your stomach and LES.
- Exercise earlier in the day: Boosts digestion, improves sleep quality, and supports weight management.
- Minimize stress: Chronic anxiety worsens reflux—try deep breathing, journaling, or walking to manage it naturally.
Explore more lasting strategies in our foundational guide to GERD lifestyle changes that actually work.
Establishing Your Own GERD-Safe Sleep Routine

There’s no one-size-fits-all for GERD, especially when it comes to sleep. It took me weeks of experimenting to find a rhythm that really worked—and some days still throw me curveballs. But once I found my groove (early dinner, chamomile tea, elevated sleeping, left-side position), I started waking up refreshed instead of wrecked.
Here’s a Sample Routine You Can Try:
- 6:30 p.m. – Eat a GERD-safe dinner
- 7:00 p.m. – Take a light walk or stretch
- 8:00 p.m. – Turn off blue light; dim the room
- 8:15 p.m. – Journal, read, or do a calming activity
- 8:45 p.m. – Sip warm herbal tea (no mint)
- 9:00 p.m. – Brush teeth, change into loose sleepwear
- 9:15 p.m. – Get into bed with head elevated, sleep on left side
This isn’t a rigid checklist, just a rhythm to experiment with. The key is to listen to your body and tweak as needed. And always keep an eye on how symptoms shift with even small adjustments—you’ll be surprised what can help.
Your Sleep, Your Gut, Your Health

Sleep should be restorative, not a nightly battle with acid. From my own experience—and the hundreds of GERD patients and readers who’ve shared their wins—your bedtime habits are one of the most powerful, low-cost tools you have to control reflux naturally.
Start small. Stick to what works. And remember: consistency beats perfection.
For more in-depth strategies on managing GERD symptoms overall, from diet to triggers, be sure to visit our comprehensive guide here: Managing Acid Reflux for a Healthier Life.

Camellia Wulansari is a dedicated Medical Assistant at a local clinic and a passionate health writer at Healthusias.com. With years of hands-on experience in patient care and a deep interest in preventive medicine, she bridges the gap between clinical knowledge and accessible health information. Camellia specializes in writing about digestive health, chronic conditions like GERD and hypertension, respiratory issues, and autoimmune diseases, aiming to empower readers with practical, easy-to-understand insights. When she’s not assisting patients or writing, you’ll find her enjoying quiet mornings with coffee and a medical journal in hand—or jamming to her favorite metal band, Lamb of God.